Local News
Chief Executive Officer of Simkin Centre Laurie Cerqueti assesses how things have changed more than six months into the pandemic

By BERNIE BELLAN As part of our continued commitment to reporting on how various agencies within the Jewish community are functioning during these exceptionally difficult times, from time to time we’ve been speaking with the heads of agencies that are directly involved with the senior population of our community.
We recently spoke with Laurie Cerqueti (pronounced Cherqueti, by the way), who’s now been in her role as CEO of the Simkin Centre for 19 months. Naturally, given all that’s happened, we wondered whether she had ever experienced anything nearly as difficult as what she – and the rest of the 250 staff at the Simkin Centre have been experiencing these past six months.
“I graduated from nursing in 1994,” Laurie said, “but nothing that I’ve ever done before comes close to what we’ve been going through these past six months.” (Prior to becoming CEO of the Simkin Centre, Laurie had been CEO of Meadowood Manor in Winnipeg.)
When I spoke with Laurie early in May – a month and a half after the lockdown of all Personal Care Homes in Manitoba had been put into effect, she described all the extra requirements that had been placed on PCH’s, including having to severely restrict access to the building; extra sanitation procedures; training of almost all staff in feeding and swallowing assistance; and so much more.
Despite the increased burdens that were placed on all PCH’s in the province, the only additional funding from the Provincial Government came in the form of “money to ensure facilities are in line with revised Manitoba Fire Code requirements, including provision of fire suppression systems and increased fire separation enhancements.”
In my May report on the Simkin Centre I noted the concern that Laurie had back then that, while PCH’s were going to have to shoulder extra financial burdens, there would be no additional assistance forthcoming from the Province:
“What about the financial situation for the Simkin Centre?” I wondered. “How different is it as a result of the pandemic?”
“There are a number of large costs for equipment and supplies – right when it started happening,” Laurie answered, “and there are ongoing costs.”
“And you mean Simkin will have to assume responsibility for those costs – and not the province?” I asked.
“I’m not confident that the province will fund partially or fully any of this,” Laurie said.
“Really – wow!” I said. “You mean it’s all going to fall on to the Personal Care Homes themselves to fund?”
“It could,” Laurie said. “I’m not confident”(that the province will provide the funding).
She added that, in addition to the extra costs imposed on PCH’s for equipment and supplies, “there are all these new rules – if you’ve traveled, you can’t come to work for 14 days; if you have any symptoms you have to go get swabbed, and then you have to have the A-OK, you can come back to work; or people that have pre-existing conditions aren’t able to work. So there are increased staffing costs that we are incurring.”
As it turned out, there wasn’t any more money made available to hire extra staff – even though workers at PCH’s were advised not to report for work if they had the slightest suspicion they might be sick. Further, the practice of workers moving between different PCH’s to fill vacant shifts was no longer allowed (quite understandably – in order to minimize the chances of community transmission of the virus).
In July, Julie Turenne-Maynard, executive director of MARCHE — The Manitoba Association of Residential and Community Care Homes for the Elderly — reported that the COVID-19 pandemic was “shining a spotlight on long-term care across the country and highlighting the consequences of a 10-year funding freeze in Manitoba.”
She said that “while Manitoba’s personal care homes have been largely fortunate in the fight against COVID-19 (and, as we’ve all seen since then, that assessment sadly proved quite wrong as PCH’s have been hit with outbreaks of the virus.) they have been chronically underfunded, despite increasing costs and needs from residents.”
Over the past 10 years, Turenne-Maynard noted, “dietary expenses at homes operated by MARCHE’s members have increased by 36 per cent and the cost of incontinence supplies increased by 50 per cent.”
Further, in the case of the Simkin Centre, the spiraling cost of kosher food – as we have noted many times before in this newspaper, has only added to the financial burden of the Jewish Personal Care Home.
Yet, despite all the pressures that the Simkin Centre has been facing, when I asked Laurie how she would describe morale among staff at the home, she said “staff morale has been very good to excellent”.
Laurie described the many ways in which members of the boards of the Simkin Centre Home Board and Foundation Board and residents’ relatives have gone above and beyond in attempting to express their appreciation to the staff. For instance, there have been weekly treats provided to staff – paid for by individual board members, residents and family members (with occasional donations from organizations such as the Gwen Secter Centre); t-shirts emblazoned with the Simkin Centre logo and the words “Simkin Strong” or #simkincares on the back; and various activities intended to boost morale.
You can read more about what the Simkin Centre has been doing to keep spirits up among both staff and residents in the Simkin Centre newsletter that is in this issue. You can also follow Simkin Centre activities on their very colourful Facebook page, or sign up to receive their weekly e-newsletter “The Simkin Star” http://eepurl.com/gVT8Q1
Despite the upbeat tone in Laurie’s voice though, I had to ask some tough questions about the toll that the pandemic has taken on residents – both physically and emotionally.
I wondered, for instance, whether there has been any noticeable increase in the number of deaths at the Centre of late?
“There have been more deaths recently than what we usually experience,” Laurie said. “Whether it’s a result of loneliness, it’s hard to say, but over the past few months there is no doubt there have been more deaths here than there would have been normally’ (but she adds that none of the deaths are either COVID related or have anything to do with the care residents receive.)
I wondered whether the loosening the rules governing visits by family members has had any noticeable effect on residents’ moods? (Until July, no family members were allowed into the actual building. You probably recall the heart-rending stories – and pictures – of residents trying to communicate with family members on Facetime or by looking through windows.)
Laurie answered that staff continue to find creative ways to keep residents busy, having fun, and remaining connected to family and faith. Whether this is through FaceTime visits (which has actually connected residents with family members that they otherwise would not have ever connected with), drive-by parades, virtual Passover and High Holiday services or other socially distanced programming.
While it’s certainly an improvement now that each resident is allowed to have visits from two family members, the fact that it always has to be the same two family members who are allowed inside has made it difficult for many families to decide who the two indoor visitors will be.
And, although outdoor visitation has been made available at the Simkin Centre – under strict conditions, now that the weather has gotten colder, those visits will be coming to an end. Plans are underway to determine and renovate a suitable space for visiting during the winter months, Laurie noted.
Given what Laurie told me about the higher than average number of deaths of late in the Simkin Centre, I asked whether there are some vacant beds?
Laurie did say that, while there are some vacancies, “a lot more people in general who are paneled (the process whereby someone is allowed to move into a PCH) are not coming” to the Simkin Centre – or to any other PCH for that matter. The honest to god truth is that so many seniors are terrified at the prospect of having to go into a PCH and subsequently be removed from their families while the pandemic rages. Of course, that places enormous extra burdens on the families of seniors who would otherwise be candidates for admission into a PCH – it goes without saying.
It’s also important to note that, as average life expectancy has increased, the individuals who do reside in PCH’s are much older than what was the typical case not too long ago.
“From 15 years ago to what we see now there are so many more residents who require a much higher level of care,” Laurie observed, while noting once again that there has been no concomitant increase in government funding for PCH’s.
I suggested that I could ask readers to bear in mind the increased financial obligations of the Simkin Centre – and perhaps consider making a donation.
Despite the inevitable stress that anyone who’s involved in health care these days must be feeling, Laurie Cerqueti still ended our conversation by saying that “I really like being associated with the Jewish community and Jewish personal care home.”
I suggested that maybe it’s because Jews and Italians are so alike in so many ways. (My wife and I are often mistaken for Italians when we travel.)
“I’m not Italian myself,” Laurie laughed, “but when you’ve been married to an Italian for 25 years you might as well be.”
Local News
Thank you to the community from the Chesed Shel Emes

We’re delighted to share a major milestone in our Capital Campaign, “Building on our Tradition.” Launched in November 2018, this campaign aimed to replace our outdated facility with a modern space tailored to our unique needs. Our new building is designed with ritual at its core, featuring ample preparation space, Shomer space, and storage, creating a warm and welcoming environment for our community during times of need.
We’re grateful to the nearly 1,000 generous donors who contributed over $4 million towards our new facility. A $750,000 mortgage will be retired in November 2025, completing this monumental project in just seven years.
We’re also thrilled to announce that our Chesed Shel Emes Endowment Fund has grown tenfold, from $15,000 to $150,000, thanks to you, the Jewish Foundation of Manitoba’s FundMatch program, and Million Dollar Match initiative in 2024. Our fund helps ensure that everyone can have a dignified Jewish funeral regardless of financial need.
As we look to the future, our goal remains to ensure the Chevra Kadisha continues to serve our community for generations to come. Our focus now shifts to replenishing our savings account and growing our JFM Endowment fund.
We’re deeply grateful for your support over the past several years.
It’s our privilege to serve our community with care and compassion.
With sincere appreciation,
Campaign cabinet: Hillel Kravetsky, Gerry Pritchard, Stuart Pudavick,
Jack Solomon, and Rena Boroditsky
Murray S. Greenfield, President
Local News
Winnipeg Beach Synagogue about to celebrate 75th anniversary

By BERNIE BELLAN (July 13) In 1950 a group of cottage owners at Winnipeg Beach took it upon themselves to relocate a one-room schoolhouse that was in the Beausejour area to Winnipeg Beach where it became the beach synagogue at the corner of Hazel and Grove.
There it stayed until 1998 when it was moved to its current location at Camp Massad.
On August 2nd members of the synagogue will be holding a 75th anniversary celebration.
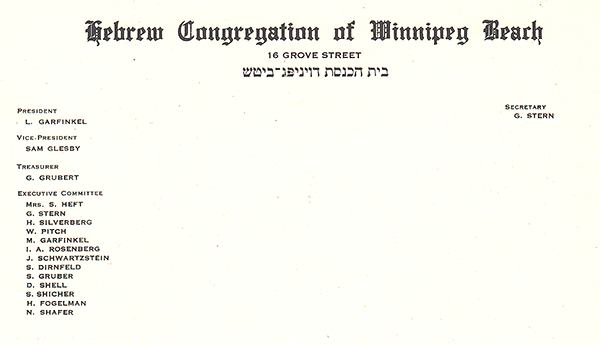
As part of the celebration anyone who is a descendant or relative of any of the original members of the first executive committee (as seen in the photo here) is invited to attend the synagogue that morning.
If you are a relative please contact Abe Borzykowski at wpgbeachshule@shaw.ca or aborzykowski@shaw.ca to let Abe know you might be attending or for more information about the 75th anniversary celebration.
We will soon be publishing a story about the history of the beach synagogue, which is something I’ve been writing about for over 25 years.
Local News
Vickar Family cuts ribbon on new Tova Vickar and Family Childcare Centre

By MYRON LOVE In the words of Larry Vickar, the Shaarey Zedek’s successful Dor V’ Dor Campaign “is not only a renewal of the synagogue but truly a renewal movement of Jewish life in our community.”An integral part of that renewal movement was the creation of a daycare centre within the expanded synagogue. On Monday, June 23, Larry and Tova Vickar cut the ribbon, thereby officially opening the Tova Vickar and Family Childcare Centre in the presence of 100 of their family members, friends and other supporters of the project.
The short program preceding the morning ribbon-cutting began with a continental breakfast followed by a welcome by both Fanny Levy, Shaarey Zedek’s Board President, and Executive Director Dr. Rena Secter Elbaze. In Elbaze’s remarks, she noted that Larry and Tova wanted their family (including son Stephen and family, who flew in from Florida) and friends at the event to celebrate the opening of the Tova Vickar and Family Childcare Centre, “not because of the accolades, but because, as Larry put it, he hopes that their investment in the congregation will inspire others to do the same.”
“When Larry and I spoke about what this gift meant to him and the message he wanted people to take away,” she continued, “I couldn’t help but connect it to the teachings of Reb Zalman Schachter-Shalomi whose book – Age-ing to Sage-ing – changes the whole way we look at the concept of ageing and basing it on our ancestral teachings.”
She explained that his concept of “Sage-ing” is based on three key ideas – Discover your meaning and purpose; accept our mortality and think about the legacy you want to leave.
“Larry spoke about these exact concepts when we met,” she said.
Elbaze also noted the presence of Shaarey Zedek’s newly-arrived senior Rabbi Carnie Rose, former Rabbi Alan Green, and area MLAs Mike Moroz and Carla Compton.
Larry Vickar expressed his great appreciation for all those in attendance. “Tova and I are deeply moved to stand here with you today for this important milestone in our community”, he said. “We are grateful to be surrounded by all of you, the people we care about, our family and friends… you who have touched our lives and played some part in our journey.”
